UK EM Field Notes #10
Silver trauma, the STUMBL score, pneumoperitoneum, tribalism
Chest injuries in silver trauma (calculate a STUMBL score!)
Chest wall injuries in older patients are common, and associated with significantly higher morbidity/mortality than younger patients.
CT (with contrast) is always the investigation of choice. It’s really tough to recognise rib fractures and lung contusions on CXR alone (up to 50% of rib fractures missed).
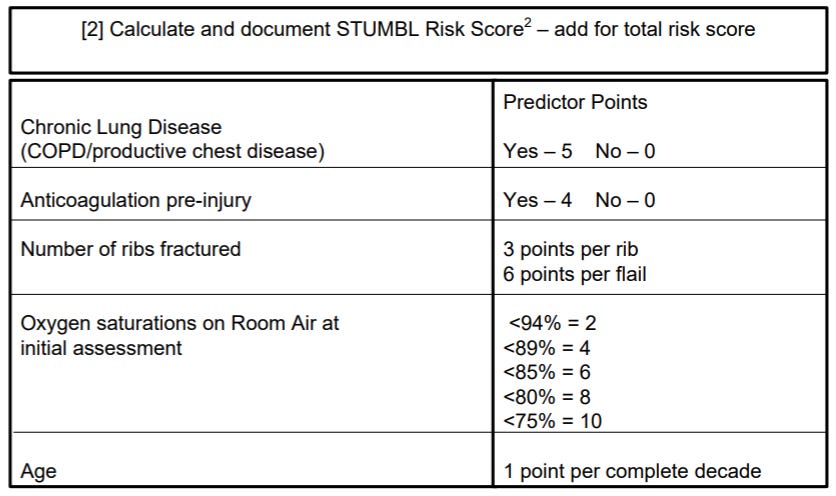
CT is essential to accurately calculate the STUMBL score (Score for Trauma in the Elderly with Blunt Thoracic Injury).
The STUMBL score is a risk stratification tool used to predict complications who have sustained blunt chest trauma. It helps guide decisions around admission, observation, escalation, and pain management.
Pain management is crucial to get on top of early. If the patient can’t take a deep breath or cough due to pain, they are a sitting duck for rapid deterioration.
All elderly patients admitted with multiple rib fractures should be considered for regional anaesthesia (serratus anterior block or erector spinae block).
At our place we have a superb local rib fracture guideline which we must remember to refer to when considering all the above.
Severe chest wall injuries including flail chests, injuries causing respiratory compromise, or where pain control cannot be achieved should be discussed early with the MTC.
Always be mindful of tension pneumothorax
In a patient with a known traumatic pneumothorax, an unrecordable blood pressure should prompt immediate consideration of a tension pneumothorax... even if none of the other physiological markers have changed much. Be very careful labelling it “machine error”.
If in doubt:
Immediately escalate.
Perform chest decompression using open thoracostomy (preferred over needle decompression as lower failure rate… though if you don’t have the skillset do a needle decompression).
Insert a chest drain through the open thoracostomy.
Pneumoperitoneum is bad
In trauma patients, pneumoperitoneum almost always means some sort of badness.
It can be a result of air tracking from a pneumothorax through one/more of the hiatuses (holes) of the diaphragm… but first you should always think perforated hollow viscus (stomach, intestine, gallbladder, etc).
We know that CT frequently misses bowel injuries in blunt trauma, as is detailed here in the World Society of Emergency Surgery guidelines on blunt and penetrating bowel injury (2022).
Pneumoperitoneum (on erect CXR or CT) should prompt an immediate trauma call with clear input from the on-call surgical team +/- discussion with the MTC.
Breaking down tribal barriers
An MDT approach to complex presentations like silver trauma (where multiple pathologies often coexist) is critical. This is especially true when diagnostic uncertainty or ambiguity exists (e.g. when a CT report is unclear/inconclusive).
Ultimately, it won’t be uncommon for silver trauma patients to end up on the medical take. It is crucial that acute medical colleagues feel empowered to revisit/re-discuss these cases with the ED consultant or registrar in charge (especially when the clinical picture evolves), with the potential for plans/dispositions to be changed.
Frail fallers often don’t declare themselves as “trauma” patients initially. Therefore, it is entirely acceptable for trauma calls can be put out even if the patient has been in the department for some time… or even after they’ve been moved to the medical ward. Senior input is clearly key when making a decision like this.
We should strive to view the particularly complex cases as an opportunity to learn from colleagues from neighbouring specialties. The more dialogue between teams, the better the outcomes for patients.
Cheers all,
Robbie
@robbielloyd.bsky.social